 A bump that extends on the side of the big toe may indicate a bunion. It is considered to be a deformity, and a common cause can be from wearing shoes that do not have adequate room for the toes to move freely in. Additionally, genetics can play a significant role in developing a bunion. Mild relief may be found when larger shoes are purchased, and it may help to wear a protective covering over the top of the bunion. In severe cases, orthotics can be prescribed, and therapy techniques may be suggested. If you notice a bony protrusion on the side of the big toe, it may be a bunion, and it is strongly suggested that you seek treatment from a podiatrist.
A bump that extends on the side of the big toe may indicate a bunion. It is considered to be a deformity, and a common cause can be from wearing shoes that do not have adequate room for the toes to move freely in. Additionally, genetics can play a significant role in developing a bunion. Mild relief may be found when larger shoes are purchased, and it may help to wear a protective covering over the top of the bunion. In severe cases, orthotics can be prescribed, and therapy techniques may be suggested. If you notice a bony protrusion on the side of the big toe, it may be a bunion, and it is strongly suggested that you seek treatment from a podiatrist.
If you are suffering from bunion pain, contact Dr. Lubrina Bryant of District Podiatry, PLLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
Symptoms
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Washington, D.C . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
 A corn is an area of skin that develops in a circular shape and is often found on the bottom of the foot or between the toes. It typically forms as a result of excess friction that can come from wearing shoes that do not fit correctly. Additionally, a corn can develop on the inside of the heel from existing medical conditions that can include flat feet. Hard corns can develop on top of the toes or on the sole of the foot. A corn that is found between the toes is referred to as a soft corn and can cause pain and discomfort. Relief may be found when the feet are washed and dried thoroughly, and it may also help to file the corn with a pumice stone. If you have a corn that is hindering daily activities, it is strongly advised that you consult with a podiatrist who can treat this condition properly.
A corn is an area of skin that develops in a circular shape and is often found on the bottom of the foot or between the toes. It typically forms as a result of excess friction that can come from wearing shoes that do not fit correctly. Additionally, a corn can develop on the inside of the heel from existing medical conditions that can include flat feet. Hard corns can develop on top of the toes or on the sole of the foot. A corn that is found between the toes is referred to as a soft corn and can cause pain and discomfort. Relief may be found when the feet are washed and dried thoroughly, and it may also help to file the corn with a pumice stone. If you have a corn that is hindering daily activities, it is strongly advised that you consult with a podiatrist who can treat this condition properly.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Dr. Lubrina Bryant of District Podiatry, PLLC. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Washington, D.C . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
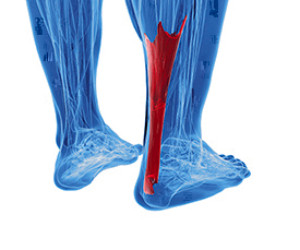 The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
The Achilles tendon connects the heel to the calf muscles. It is located in the back of the leg, near the foot, and is responsible for the ability to point and flex the foot. An injury can cause the Achilles tendon to become ruptured or injured, and this generally causes severe pain and discomfort. Some of the symptoms that many patients can experience include sharp pain at the time of the injury, bruising, swelling, and it is often difficult to walk. This type of injury can happen as a result of participating in running and jumping movements, or if a new activity begins suddenly. Effective treatments can include wearing a brace or cast as the healing process occurs, and in severe tears, surgery may be necessary. If you have pain in your calf, it is strongly advised that you speak to a podiatrist as quickly as possible who can treat an Achilles tendon injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Lubrina Bryant of District Podiatry, PLLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Washington, D.C . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
 Having dry skin is one of the many factors that can result in the formation of cracked heels. Those who have biomechanical issues that increase the pressure put on the heel, may be more likely to experience cracked heels. Being obese can also create an increase in pressure put on the heels, as the feet are responsible to carry the extra weight. This causes a loss of suppleness in the pads of the feet. Due to this lack of flexibility and increased pressure, cracks and deep fissures can form on the heels. Wearing open back shoes can also be a risk factor for developing cracked heels, as these types of shoes may cause the fat pads in the heel to expand sideways, creating cracks. Certain skin conditions, such as psoriasis, eczema, and fungal infections, can increase dryness of the skin thus leading to cracks or fissures. In severe cases, cracked heels may cause bleeding. If you feel you have developed cracked heels, please visit a podiatrist for professional care and treatment.
Having dry skin is one of the many factors that can result in the formation of cracked heels. Those who have biomechanical issues that increase the pressure put on the heel, may be more likely to experience cracked heels. Being obese can also create an increase in pressure put on the heels, as the feet are responsible to carry the extra weight. This causes a loss of suppleness in the pads of the feet. Due to this lack of flexibility and increased pressure, cracks and deep fissures can form on the heels. Wearing open back shoes can also be a risk factor for developing cracked heels, as these types of shoes may cause the fat pads in the heel to expand sideways, creating cracks. Certain skin conditions, such as psoriasis, eczema, and fungal infections, can increase dryness of the skin thus leading to cracks or fissures. In severe cases, cracked heels may cause bleeding. If you feel you have developed cracked heels, please visit a podiatrist for professional care and treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Dr. Lubrina Bryant from District Podiatry, PLLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Washington, D.C . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Our feet are arguably one of the most important parts of the body. When it comes to health and beauty routines, the feet and toenails are usually ignored. You should always practice proper footcare to avoid any fungal infections or ailments that can not only ruin the appearance of your feet, but also cause pain. Ignoring any foot problems could potentially lead to an expensive doctor’s visit.
The most important step in proper foot care is to wash your feet daily. You should wash them with soap and water. Doing this will cleanse your feet of dirt, sweat and bacteria. It is crucial that you clean between the toes and pat your feet dry with a towel afterward. Your toenails are also an important part of the feet and you may find that they get dirtier in the summer when you wear sandals. It is important that you practice proper toenail care in addition to cleaning the rest of your feet. When trimming your nails, you should always trim straight across instead of in a rounded shape. Trimming in a curved shape may lead to ingrown toenails.
Moisturization is also important for foot care, and you should be moisturizing your feet every day. The best way to prevent dry feet is to rub lotion or petroleum jelly on your clean feet at night and put socks over them. In the morning, your feet should be soft and moisturized.
Another crucial step in proper foot care is to wear the right shoes for whichever activity you are going to partake in. In warmer weather, you should wear shoes that allow your feet to breathe. It is best to avoid shoes such as flip-fops that do not provide arch support. Tight shoes may also be harmful, and they may even cause you to develop bunions.
If you plan on taking a shower in a public area, you should be especially careful, so you do not pick up any fungi. Showers are prone to harboring different types of bacteria and fungi. You should always wear shower shoes or flip flops when walking around in locker rooms and public showers. Avoid sharing shoes with other people because this is another way that fungus may be spread.
If you are experiencing any problems with your feet you should speak with your podiatrist to determine the best method of treatment for you.